Diagnostics
Hypothermia
Elderly male patient with history of mental illness, homelessness, alcoholism, hypopituitarism, hypothyroidism, hypoadrenalism, CVA presents with hypothermia. Patient found submerged in water with head trauma. Received aggressive fluid resuscitation en route. Temperature < 35 C on exam.
Atrial fibrillation and J wave in severe hypothermia. Credit: WikiSysop.
Severity
Mild (32.2-35 C): Hypertension, tachycardia, tachypnea, hypovolemia, shivering, ataxia, apathy, increased urine output.
Moderate (28-32.2 C): Bradycardia, bradypnea, hypotension, decreased level of consciousness, pupillary dilation, hyporeflexia. No shivering noted.
Severe (< 28 C): Non-responsive with non-reactive pupils, apnea, crackles on lung exam, oliguria. EKG shows ventricular arrhythmia, J-waves. Decreased activity on EEG.
Labs
Measure temperature with low-read rectal thermometer
Obtain fingerstick glucose, CBC, CMP q4h, PT/PTT/INR, TSH, Free T4, EtOH level, urine drug screen
Consider scheduling cosyntropin stimulation test after resuscitation if hypoadrenalism suspected
Treatment: Do not abandon resuscitation efforts until core temperature > 32.2 C
Mild hypothermia and hemodynamically stable moderate hypothermia
Remove wet clothing
Passive rewarming: Move to warm environment, insulate, administer warmed liquids PO
Hemodynamically unstable due to moderate/severe hypothermia
Insulate with Bair Hugger, start D5NS at 40 C
Avoid NG tube placement due to risk for precipitating AFib
Consider surgical c/s for active rewarming via closed thoracic lavage
Cardiac arrest
Follow AHA resuscitation guidelines, but do not defibrillate unless VFib is present.
VFib on EKG: One time trial of defibrillation. If unsuccessful, do not repeat until core temperature > 30 C.
Comorbidities
Monitor for hemorrhage
Replete glucose, electrolytes PRN
Suspected alcoholism and/or positive EtOH: Administer empiric thiamine 250 mg IV x 3 days followed by 100 mg PO x 1 month
Confirmed adrenal insufficiency: Administer empiric steroid therapy
Patient advised to prevent future episodes by wearing layers and carrying a winter survival kit
Notes
Etiology
Cold exposure (e.g. homelessness) +/- concomitant alcohol use is the most common cause of hypothermia
Hypopituitarism, hypothyroidism, hypoadrenalism, and CVA may result in temperature dysregulation
Aggressive hydration is a common cause of iatrogenic hypothermia
Physiology
Severe hypothermia is associated with pulmonary edema (crackles)
Cold diuresis: Kidneys lose concentrating ability
Hypothermia may disrupt enzymatic reactions in clotting cascade despite normal PT/PTT/INR results
Electrolyte levels may change rapidly during resuscitation; this is especially true for potassium
J waves are positive deflections occurring at the junction between the QRS complex and the ST segment
Treatment
Most clinical thermometers only measure as low as 34.4C (94F)
Core temperature afterdrop: Phenomenon in which pt clinically worsens when circulation resumes and cold blood returns to heart; minimize by utilizing passive rewarming when possible
Closed thoracic lavage: Two thoracostomy tubes placed and warmed saline circulated through thoracic cavity
Severe Asymptomatic Hypertension
Patient presents with hypertensive crisis. No subjective complaints. Denies headache, visual disturbance, lightheadedness, nausea, epistaxis, dyspnea, chest pain, palpitations, oliguria. No h/o coronary artery disease, heart failure, CVD, chronic kidney disease, DM, obstructive sleep apnea, EtOH/stimulant abuse. BP >180/>110. RR, SPO2 WNL. No neurologic deficits, JVD, arrhythmia, new onset heart murmur, pulmonary rales on exam.
Repeat blood pressure 30 minutes after initial measurement
Blood pressure remains elevated
Obtain CMP and compare results to previous labs: Admit to hospital if changes suggest end organ damage, e.g. AKI, AST or ALT > 2x upper limit of normal
Outpatient treatment for patients without evidence end organ damage:
No h/o HTN: Start home BP monitoring and f/u in 2-4 weeks
H/o HTN: Adjust hypertensive medications
Severe HTN with Mild Symptoms
Pt with h/o HTN presents with hypertensive crisis. Reports new onset headache, lightheadedness, nausea, epistaxis, shortness of breath, palpitations, anxiety. BP >180/>110.
Repeat BP 30 min after initial BP measurement
Obtain BMP, U/A to assess for end-organ injury; compare with previous labs
Treatment
Agent
No h/o asthma, HF, heart block, bradycardia: Administer labetalol 20 mg IV
Labetalol contraindicated: Administer hydralazine 10 mg IV
Re-evaluate
Symptoms improve with short acting HTN Rx: Start/adjust HTN Rx and f/u in 1 week
Symptoms do not improve with short acting HTN Rx and no indication of end-organ damage on labs; start/adjust hypertensive tx and f/u in 1 week
Concerns about medication adherence and/or evidence of pulmonary rales, JVD, arrhythmia, new onset heart murmur, neurologic deficits: Admit for inpatient management
Notes
Systolic > 240 mmHg or diastolic > 130 mmHg may benefit from hospitalization
End organ damage
There is no consensus or guidelines for the definition of end-organ damage criteria in severe hypertension. AKI is commonly considered a marker for end-organ ischemia and the KDIGO definition is provided below. LFT and urine criteria were adopted from preeclampsia management that also assess for end-organ damage.
AKI is defined as any of the following:
Increase in serum creatinine (SCr) by ≥ 0.3 mg/dl within 48 hours
Increase in SCr to ≥ 1.5 times baseline within previous 7 days
Urine volume < 0.5 ml/kg/h for 6 hours
White Blood Cells
Leukocytopenia
Pancytopenia
Production
Iatrogenic, e.g. chemotherapy
Infection
Viral
Epstein-Barr virus (EBV)
Hepatitis
HIV
Tuberculosis
Autoimmune
Rheumatoid arthritis
Systemic lupus erythematosus
Sarcoidosis
Malignancy
Multiple myeloma
Leukemia
Consumption
Splenomegaly (multiple etiologies)
Disseminated intravascular coagulation
Neutropenia
Definitions
Neutropenia: ANC < 1500 cells/microL
Severe neutropenia (ANC < 500): Initiate neutropenic precautions (see below)
Agranulocytosis: ANC < 200 cells/microL
Etiologies
Benign ethnic neutropenia (most common)
Nutritional deficiency, e.g. B12, folate
Viral illness
Liver cirrhosis
Autoimmune disorder
Pancytopenia (see above)
Medication-induced, e.g. antibiotics, anti-inflammatories including NSAIDs, clozapine, tricyclic antidepressants, thyroid medications, sulfonylureas
Source: Minnesota Hospital Association
Leukocytosis
Lymphocytosis
More coming soon
Neutrophilic Leukocytosis
Pt with h/o smoking, irritable bowel disease, hepatitis, rheumatic disease, granulomatous disease, vasculitis, sickle cell s/p splenectomy presents with new onset neutrophilia. Reports recent sick contacts, febrile seizures, panic attacks, surgery. Denies chronic fever, fatigue, weight loss, night sweats, pregnancy. Medications include corticosteroids, beta agonists, lithium, epinephrine, colony-stimulating factors. Fever on exam. No bruising, lymphadenopathy, splenomegaly noted.
Labs
Neutrophils >60% and 7,000/mm^3; obtain repeat CBC to confirm result
Obtain peripheral smear
Evaluate for hemolytic anemia, ITP
Rule out presence of blasts
Obtain ESR, CRP, ANA, blood cultures
Consider lumbar puncture
Consider empiric antibiotics
Notes
Neutrophilia may be normal in patients with h/o splenectomy, smoking
Congenital conditions such as Down Syndrome may result in neutrophilia
Neutrophilia etiologies include physiologic stressors including pregnancy, bone marrow stimulation, acute infection
Factors that increase concern for malignancy include chronic fever, fatigue, weight loss, night sweats
Monocytosis
Infectious, e.g. EBV, tuberculosis
Autoimmune disease
Chronic myelogenous leukemia
Thrombocytopenia
Pt with h/o alcohol-induced liver disease, leukemia, mechanical heart valve presents with thrombocytopenia. Reports recent tick-bite, fever/night sweats, unintended weight loss, weakness/fatigue, easy bruising. Currently undergoing chemotherapy. Recently received MMR, varicela, and influenza vaccines. Medications include NSAIDs, furosemide, ranitidine. Family h/o thrombocytopenia. Slapped-cheek rash, mucosal petechiae, lymphadenopathy, heart sounds with mechanical click, ascites, hepatosplenomegaly, jaundice on exam. No active bleeding noted.
Labs
Repeat CBC confirms thrombocytopenia
CMP shows elevated alkaline phosphatase and AST:ALT >2
Obtain blood smear, GGT, hepatitis panel, HIV ELISA
Consider obtaining rickettsial viral panel, bone marrow biopsy
Treatment
Stop NSAIDs, furosemide, ranitidine
Concern for alcohol withdrawal; start CIWA protocol
Platelet count < 50,000/microliter with active bleeding: Transfuse 1 apheresis unit of platelets
Patient’s hematologist-oncologist notified about current condition
Counseling
Pt advised to stop drinking alcohol
Pt counseled that if his condition is medication-induced, it will likely resolve in 7-14 days
Notes
Risk factors and conditions associated with thrombocytopenia
Viral illness including:
HIV
Hepatitis B/C
Parvovirus B19
Herpesviridae: VZV, EBV, CMV
Tropical: Dengue fever, malaria
Alcohol abuse and/or chronic liver disease
Mild to moderate thrombocytopenia due to decreased platelet production
May be associated with GI bleeding
Labs may show macrocytic anemia, elevated AST:ALT, and/or elevated GGT
Marrow suppression due to malignancy/chemotherapy: Moderate to severe thrombocytopenia that generally affects all cell lines
Congenital thrombocytopenia
Iatrogenic
MMR, varicella, influenza A (H1N1) vaccines
Destruction by mechanical heart valve
Treatment
Repeat CBC to rule out in vitro agglutination
Therapy based on platelet counts (per microliter)
> 150,000: No further workup
100,000-150,000: Repeat blood work in 2-4 weeks
50,000-100,000: Trend counts until > 100,000 or < 50,000 and attempt to determine etiology
< 50,000: Consider hematology referral/consult
Immune (idiopathic) Thrombocytopenic Purpura
Acquired autoimmune disorder
Must r/o all other etiologies (see DDX)
Giant platelets on peripheral smear
For patient >60 obtain bone marrow biopsy to r/o myelodysplastic syndrome/lymphoproliferative disorders
Treatment
Indicated if acute bleeding is present or platelets <50,000
Corticosteroids = first line
IVIG and rituximab may also be used
Hypovolemic Hyponatremia - Renal Loss
Pt with h/o intracranial hemorrhage, Addison's disease presents with headache, dizziness, lethargy. Reports anorexia, weakness, fatigue, N/V, abdominal pain, diarrhea, recent diuretic abuse. Tachycardia, orthostatic hypotension, A&O x 3, normal gait on exam; no jaundice.
Collect blood/urine concomitantly: Obtain BMP, lipid panel, serum osmolality/urea, urine osmolality/sodium/creatinine
Calculated serum mOsm < 280
Urine sodium
> 40: Diagnosis confirmed
Diagnosis unclear due to urine sodium 25-40 mEq/L
Infuse 1L isotonic saline
Remeasure urine sodium in 1 hour
Diuretic abuse suspected due to urine fractional excretion urea < 35%
Schedule morning cosyntropin stimulation test
Monitor urine; advise MD if output > 100 mL/hr as this may indicate overcorrection
U/S to evaluate for IVC collapse
Treatment
Correct hyperglycemia
Stop diuretic
Start NS at maintenance
Consider salt tablets for long-term management
Obtain endocrine consult
Recent seizures or LOC: Consider ICU admission for observation/management
Notes
Etiologies
Diuretic abuse: Increases urine sodium; use urine fractional excretion of urea if suspected
Osmotic diuresis due to hyperglycemia
Addison's disease (anorexia, weight loss, weakness, fatigue)
Intracranial hemorrhage may lead to salt wasting; consider head CT
Calculations
Serum mOsm = [(sodium x 2) + (glucose / 18) + (blood urea nitrogen / 2.8)]
Urine FEU = [(serum Cr * urine urea) / (serum urea x urine Cr)] * 100
Hypovolemic Hyponatremia - Extrarenal
Pt with h/o GI fistula presents with headache, dizziness, lethargy. Reports recent vomiting, constipation, sweating, severe burns. Denies seizures, LOC. Tachycardia, orthostatic hypotension, hyperthermia, A&Ox3 on exam.
Labs
Collect blood/urine concomitantly: Obtain BMP, lipid panel, serum osmolality
Calculated serum mOsm < 280
Urine sodium < 25
Monitor urine; advise provider if output > 100 mL/hr as this may indicate overcorrection
Imaging
U/S to evaluate for IVC collapse
Obtain CT to r/o bowel obstruction
Treatment: Administer isotonic or hypertonic saline
Notes
Etiology
Vomiting/diarrhea may lead to GI sodium loss
Bowel obstruction → third spacing → hyponatremia
Serum mOsm = [(sodium x 2) + (glucose / 18) + (blood urea nitrogen / 2.8)]
Diet-Induced Euvolemic Hyponatremia
Elderly pt with h/o schizophrenia, alcoholism presents with new onset headache, lethargy, dizziness. Reports anorexia, excess beer and water consumption. Diet consists of tea and toast. No orthostatic hypotension, moist mucous membranes, no LE edema on exam.
Obtain BMP, urine sodium/osmolality/drug screen, EtOH level
Serum mOsm < 280
Urine Na > 40 mEq/L and urine osmolality < 100 mOsm/kg
U/S shows no IVC collapse
Treatment
Regular diet and restrict fluid to 500 mL less that daily urinary output; start 1.5 L fluid restriction
Suspected EtOH abuse: Start CIWA protocol and treat accordingly
Psychogenic polydipsia
Obtain EKG; restart previous psychiatric medications if QTc WNL
1:1 sit and monitor while showering
Consider social work, case management consult
Serum mOsm = [(sodium x 2) + (glucose / 18) + (blood urea nitrogen / 2.8)]
Hypernatremia
Elderly pt on hemodialysis with h/o altered mental status, DM, diabetes insipidus, and salt tablet/diuretic abuse presents with new onset vomiting, watery diarrhea, polyuria and diffuse burns. Additional symptoms include anorexia, muscle weakness, restlessness, N/V. Febrile with hyperventilation on exam.
Obtain CMP, TSH serum osmolality, urine sodium, urine osmolality, urinary uric acid
Corrected Na = measured Na + 0.024 × (serum glucose − 100)
FENA = ([Plasma Cr × urinary Na] / [plasma Na × urinary Cr]) × 100
Low threshold for head CT as hypernatremia can cause brain shrinkage with concomitant vascular rupture/intracranial bleed
Treatment
Hold amphotericin, aminoglycosides, lithium, phenytoin (Dilantin)
Concern for impaired thirst mechanism due to decreased PO intake; pt encouraged to increase PO intake
Notes
Hypernatremia is associated with increased morbidity/mortality in the inpatient setting
FENA interpretation
Prerenal < 1%
Intrinsic > 1%
Postrenal > 4%
Stress Hyperglycemia
Pt with h/o DM presents with transiently elevated blood glucose. Recent h/o CNS infection, sepsis, and ICU admission. Current temperature > 39 C.
D/c glucose containing fluids
Titrate insulin to maintain blood glucose of 140-180
Acid-Base Disturbances
Initial Approach
What is the primary derangement and is it metabolic or respiratory?
Acidosis = pH < 7.35
Respiratory: pCO2 > 40
Metabolic: pCO2 < 40
Alkalosis = pH > 7.45
Respiratory: pCO2 < 40
Metabolic: pCO2 > 40
Is the primary derangement acute/chronic and adequately compensated?
Clinical assessment and a blood gas (arterial or venous) are needed to determine etiology and degree of compensation
Respiratory acidosis
Acute
Δ PaCO2 of 1 → Δ pH 0.01
For every ↑ 10 mEq PaCO2 = ↑ 1 mEq HCO3
Chronic: For every ↑ 10 mEq PaCO2 = ↑ 3-5 mEq HCO3
Metabolic acidosis: Expected PaCO2 = (1.5 x HCO3) + 8 +/- 2
If measured PaCO2 is higher than expected, then respiratory compensation is inadequate, i.e. respiratory acidosis.
If measured PaCO2 is lower than expected, it implies underlying respiratory alkalosis.
Metabolic alkalosis: Expected PaCO2 = (0.7 x HCO3) + 21 +/- 2
If measured PaCO2 is higher than expected, it implies acute respiratory acidosis, i.e. inadequate respiratory compensation.
If measured PaCO2 is lower than expected, it implies underlying respiratory alkalosis.
Respiratory Acidosis Etiology
Central nervous system depression
Acute: Trauma, intoxication, encephalitis
Chronic: Neuromuscular disease, e.g. muscular dystrophy
Lung disease
Metabolic Acidosis Etiology
Anion gap
[Na+] - ([Cl-] + [HCO3-])
Normal anion gap ≈ 12
High Anion Gap Metabolic Acidosis (HAGMA): MUDPILES
Methanol
Uremia
Paraldehyde
Iron, INH toxicity
Lactic acidosis
Ethanol, ethylene glycol
Seizure, starvation, salicylates (aspirin)
Normal Gap Metabolic Acidosis: USED CAR
Urinary-colonic fistula
Saline
Endocrine disorders of aldosterone, e.g. Addison’s disease
Carbonic anhydrase inhibitor, e.g. acetazolamide
Alimentary (total parenteral nutrition)
Renal tubular acidosis
Etiology per Pathophysiology
HAGMA due to increased acid ingestion/production
Lactic acidosis
Hypoxia including hypovolemic, cardiogenic, and distributive (septic) shock
Systemic disease, e.g. cirrhosis, malignancy
Ketoacidosis: Starvation, Alcohol, DM (ketoacidosis = SAD)
Acid ingestion: Methanol, ethylene glycol, salicylic acid (aspirin)
Normal anion gap metabolic acidosis: HCO3 versus H+
Bicarbonate: Decreased production or increased elimination
Diarrhea
Carbonic anhydrase inhibitors
Type 2 (proximal) renal tubular acidosis
Decreased renal acid excretion
Renal tubular acidosis types 1 and 4
Additional Calculations
Osmolar gap = Measured serum OSM - [2(Na+) + (glucose/18) + (BUN/2.8)]
Normal ≈ 10 to 15
Used to help further differentiate HAGMA etiology in cases of toxic ingestion
> 10 to 15 but < 25 indicates alcohol toxicity, e.g. methanol, ethanol, ethylene glycol, propylene glycol, isopropyl alcohol
> 25 indicates methanol or ethylene glycol
Urine anion gap = [(urine Na)+(urine K)] - urine Cl
Normal ≈ 0
Negative balance indicates gut losses
Significantly elevated balance indicates chronic kidney disease or renal tubular acidosis
Acidosis Management
Metabolic
Treat underlying etiology: DKA, lactic acidosis (shock/cirrhosis/malignancy), diarrhea, CKD, toxic ingestion
Severe acidosis (pH < 7.1)
Transfer patient to ICU and assess for intubation
Initiate sodium bicarbonate at 50 to 100 mEq per day and titrate to pH > 7.3
Respiratory (hypercapnia)
Treat underlying etiology
Hypercarbia/CO2 narcosis in patient with altered mental status, RR > 25, and/or pH < 7.3:
Initial evaluation
Consider contributing etiologies (see above)
Note: Altered conscious does not usually occur until PaCO2 > 75 mmHg
Start BiPaP 12/5 at 30% FiO2
Increase FiO2 by 5% every 10 minutes to achieve to SPO2 90-93%, i.e. FiO2 30% → 25% → 40% → etc.
If pt cannot tolerate BiPaP, transfer to ICU for sedation and monitoring
Provided continued hemodynamic stability, recheck ABG after 1 hour if significant clinical improvement is noted
Intubate for any of the following
Development of hemodynamic instability
No significant improvement of clinical status and ABG values after 1 hour
Intubate for pH < 7.2
Alkalosis
Common Etiologies
Metabolic
Diuretic therapy
Gastric secretion loss (vomiting)
Respiratory
Acute: Hyperventilation (multiple respiratory etiologies)
Chronic: Pregnancy, heart failure, hepatic failure, hyperthyroidism
Treatment
Address underlying etiology, e.g. stop diuretics, control nausea, etc.
Consider administration of one of the following:
Potassium chloride if hypokalemia is present
Acetazolamide (carbonic anhydrase inhibitor) 500 mg IV x 1 dose
Hypercalcemia
Pt with h/o nephrolithiasis presents with lethargy/weakness, abdominal pain, flank pain, and confusion. Reports recent, excessive intake of vitamin D, calcium, and thiazide diuretic. Family history positive for sarcoidosis, breast cancer. HTN, irregular heartbeat, abdominal tenderness, flank pain, muscle weakness, and lower extremity edema on exam.
CMP shows corrected calcium > 10.5 mg/dL
Repeat CMP and re-evaluate serum calcium and creatinine levels
If repeat serum calcium elevated; obtain PTH level and serum ionized calcium
Obtain PTH level
PTH > 65 pg/mL: See primary hyperparathyroidism
PTH < 20 pg/mL: Obtain PTHrP, 1,25-dihydroxyvitamin D, and 25-dihydroxyvitamin D levels
Elevated PTHrP: Obtain CBC, and consider CXR, mammogram, abdominal CT, and/or serum electrophoresis
Elevated 1,25-dihydroxyvitamin D: Obtain CXR to r/o sarcoidosis, lymphoma
Elevated 25-dihydroxyvitamin D levels: Review all medications and counsel pt about vitamin D toxicity.
All levels normal: Consider obtaining TSH, serum protein electrophoresis, cortisol level, and/or vitamin A level
EKG shows peaked T waves
Treatment
Calcium < 14 mg/dL: Stop vitamin D, calcium supplementation and thiazide diuretic; encourage adequate hydration
Calcium > 14 mg/dL
Start normal saline at 250 mL/hr and adjust to maintain urine output of 100 mL/hr
Consider starting once-monthly pamidronate 90 mg IV
Notes
Corrected Ca = [0.8 x (normal albumin - patient's albumin)] + serum Ca level
PTHrP = Parathyroid hormone related peptide
Resources: https://clinicalproblemsolving.com/dx-schema-hypercalcemia/, https://www.uptodate.com/contents/diagnostic-approach-to-hypercalcemia
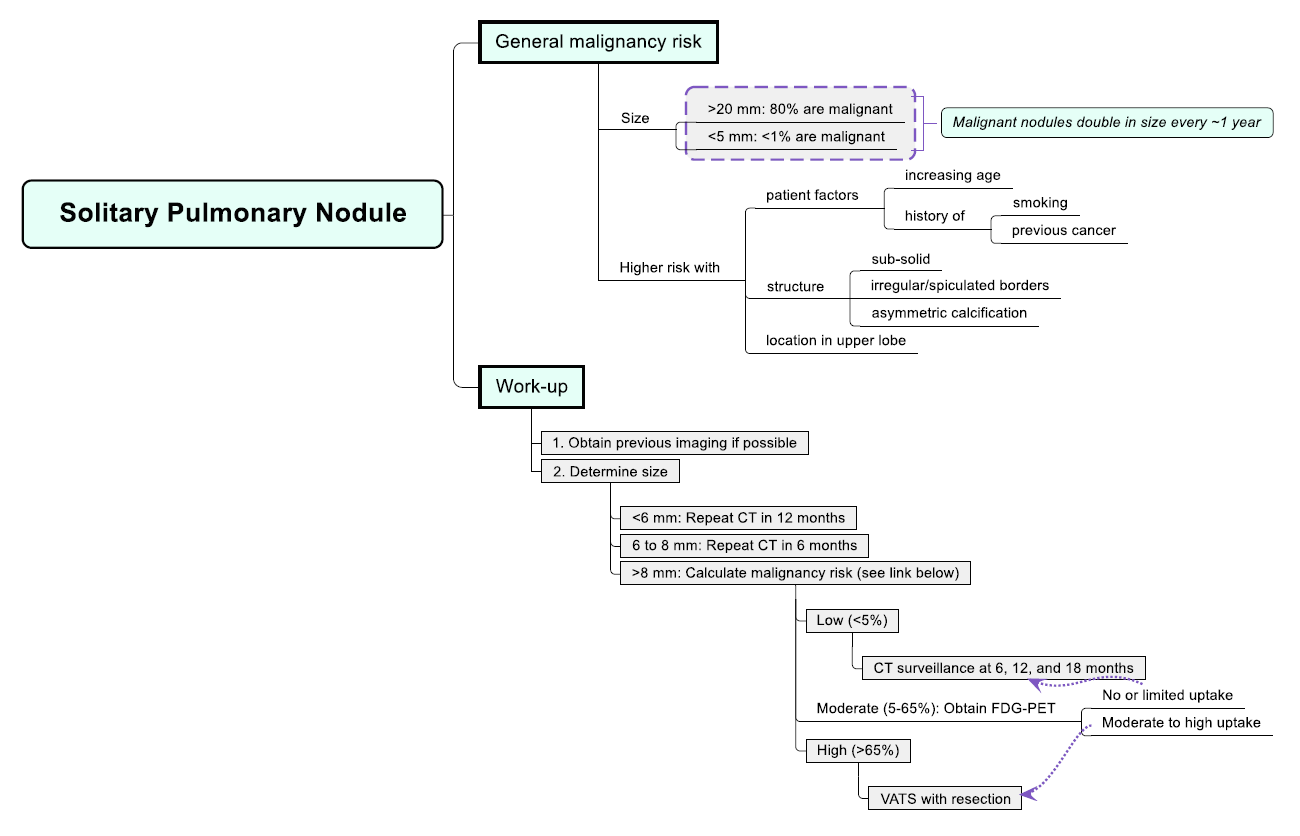
Notes
Nodules <4 mm in patients age 65 years or younger with no history of smoking or malignancy may not need follow-up imaging. The algorithm above provides a simplified and cautious approach.