Endocrine

Endocrine
Pt with h/o cerebral tumor presents with new onset hyponatremia s/p surgery. Symptoms of fever, headache, neck stiffness, SOB additionally concerning for pneumonia, meningitis. Medications include amiodarone, carbamazepine, chlorpromazine, SSRI. Denies use of diuretics, Ecstasy. Does not eat low salt diet. Fever, MMM, nuchal rigidity, pulmonary crackles, euvolemia on exam.
Labs
Serum mOsm: [(Na x 2) + (glucose / 18) + (BUN / 2.8)] < 280
Urine Na > 40 mEq/L and urine osmolality > 100 mOsm/kg
Serum BUN:Cr ratio, TSH within normal limits
Urine drug screen negative
Trial of 1L NS
SIADH indicated by decreased sodium levels s/p bolus
If urine Na > 40 mEq/L or urine Osm < 100 mOsm/kg s/p bolus, reconsider hypovolemic hyponatremia
Imaging
U/S shows no IVC collapse (euvolemic)
Consider CXR to evaluate for pneumonia
Treatment
D/c medications associated with SIADH
Fluid restrict to 1.5L daily
If no improvement with fluid restriction
Obtain ACTH stimulation test to r/o adrenal insufficiency
ACTH stimulation test negative for adrenal insufficiency: Obtain renal consult and consider starting vaptans
Pt counseled that long-term control may require loop diuretics and high salt diet
Diuretic use and low sodium diets can complicate differentiating between hypovolemic and euvolemic hyponatremia
Conditions commonly associated with SIADH
Surgery
Pneumonia
CNS insults (e.g. tumor, meningitis)
Other euvolemic hyponatremia etiologies include hypothyroidism, adrenal insufficiency, Ecstasy use
49 y/o F with h/o HTN, hyperlipidemia, recurrent miscarriages presents with chronic fatigue and cold intolerance. Reports h/o autoimmune disease, ovulatory/menstrual dysfunction, and neck irradiation. Denies currently being pregnant. ROS positive for poor concentration, depression, and diffuse muscle pain. Medications include amiodarone and lithium. Hair thinning, goiter, proximal muscle weakness, lower extremity edema, dry skin, and delayed deep tendon reflexes on exam.
TSH > 10 mIU/L with low free T4
Start levothyroxine 1.6 mcg/kg/day PO and repeat TSH testing in 6 weeks
Adjust levothyroxine dose every six weeks until TSH within reference range
Levothyroxine counseling
Take every morning on an empty stomach at least 30 minutes before food
Do not take within 4 hours of calcium, iron, and/or bile acid sequestrants (e.g. cholestyramine)
Notes
Initial workup
Fatigue and cold intolerance are the most common symptoms of hypothyroidism
May be preceded by signs/symptoms of hyperthyroidism, i.e. Hashimoto’s thyroiditis. In these cases, autoimmune destruction of the thyroid gland leads to chronic hypothyroidism.
Amiodarone and lithium may cause thyroid dysfunction
Start with TSH testing
General reference range is 0.5 < TSH < 10 mIU/L
If TSH > 5.5 mIU/L, obtain free T4
Treatment
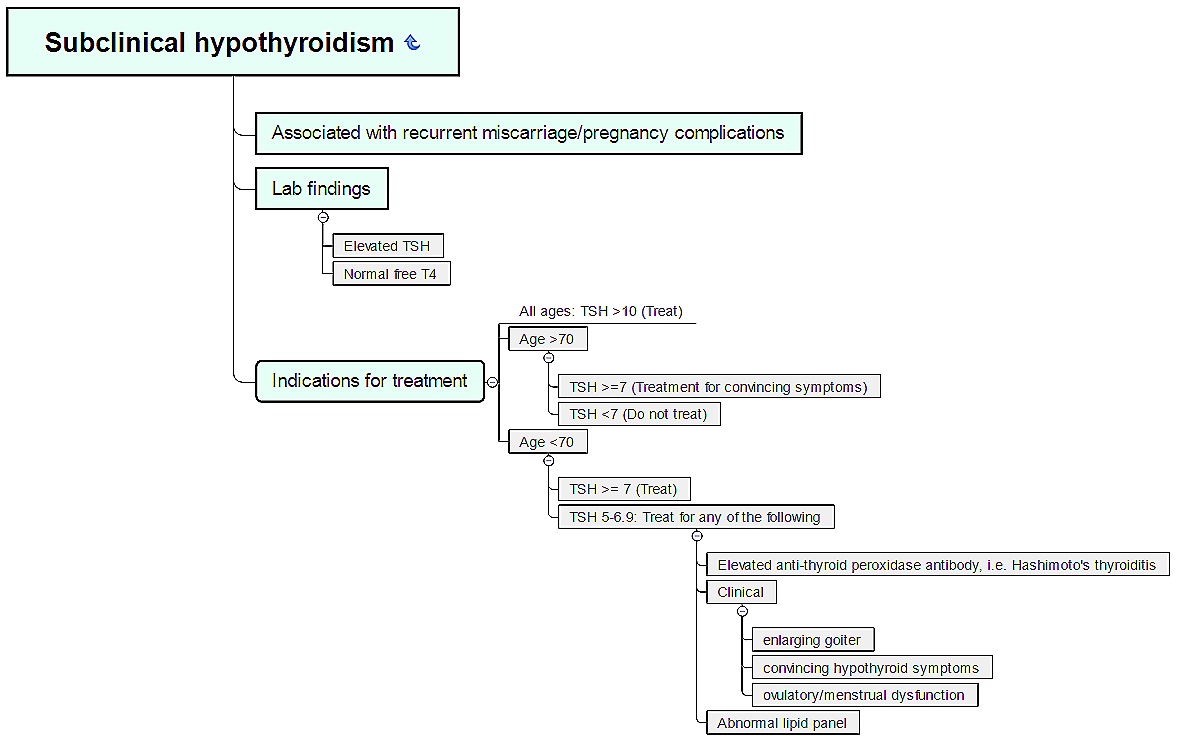
TSH < 10 mIU/L and normal free T4 indicates subclinical hypothyroidism (see vignette/chart below)
Hypothyroidism treatment depends on age, symptoms, and pregnancy status
For patients 50 or older, start levothyroxine 25 mcg daily and increase by 25 mcg every 4 weeks until TSH reaches desired range
In newly pregnant patients, increase current levothyroxine from 7 to 9 tablets weekly (e.g. two tablets on Tuesday/Thursday and one tablet as usual on other days)
TSH changes in previously stable hypothyroid patients being treated with levothyroxine:
Numerous medications may alter TSH, including SSRIs
Decreased levothyroxine absorption may occur with atrophic gastritis, chronic PPI use, and/or H. Pylori infection
69 y/o F with h/o autoimmune disease and neck irradiation presents with chronic fatigue and cold intolerance. Denies weight gain, constipation, arthralgias/myalgias, weakness, difficulty concentrating, depression. Vital signs WNL. Normal hair, thyroid, and skin on exam.
TSH 6.9 mIU/L with normal free T4
Obtain lipid panel, anti-thyroid peroxidase antibodies
Treat as indicated per laboratory results
Notes
Subclinical hypothyroidism = elevated TSH with normal free T4
Treatment depends on age, symptoms, TSH, anti-TPO antibodies, and lipid panel (see below)
Rule of 7’s: TSH 7 mIU/L or greater and
70+ y/o = treat if symptomatic
Less than 70 y/o = treat
Pregnant pt with h/o autoimmune disease presents with worsening heat intolerance, insomnia, and anxiety/restlessness. Reports recent onset diplopia, blurred vision, reduced color perception, and diarrhea. HTN, exophthalmos, goiter, periorbital edema, thyroid acropachy, pretibial myxedema, and vitiligo on exam.
TSH < 0.1 mIU/L with inappropriately elevated free T4 and total T3 levels
Positive anti-thyroid peroxidase (TPO) antibodies
Radioactive iodine uptake scan of thyroid shows high uptake with homogeneous radioactive iodine distribution
Treatment
1st trimester of pregnancy: Start Propylthiouracil 50 mg TID and titrate to appropriate TSH
After 1st trimester: Methimazole 5-120mg in divided doses; pt counseled about dose-dependent risk for agranulocytosis
Pt advised that definitive treatment will include radioactive iodine ablation vs. surgical removal of thyroid gland
Thyroid acropachy
Clubbing of fingers/toes with swelling of hands/feet; considered pathognomonic for Graves disease
Rare: Occurs in only 0.3% of patients
Anti-thyroperoxidase (TPO) antibodies are markers of autoimmune destruction of thyroid tissue may be positive in Graves disease (hyperthyroidism) or Hashimoto’s thyroiditis (hypothyroidism)
Only hyperthyroid state with high, homogeneous uptake of radioactive iodine
Elderly pt presents with new onset palpitations and heat intolerance. Reports associated sweating, tremor, and anxiety. Pt has lived in Great Lakes region her entire life, keeps Kosher, and exclusively eats garden non-processed foods flavored with sea salt. Tachycardia and lid-lag on exam.
TSH < 0.1 mIU/L with elevated free T4 and T3 levels
Radioactive iodine uptake scan of the thyroid shows high uptake with nodular radioactive iodine distribution in multiple areas of accumulation
Treatment: Trial of medications to control symptoms including
Propranolol extended release 80 mg daily
Methimazole 5 mg TID; f/u labs in 6 weeks with titration to 20 mg TID as needed to maintain TSH, free T4 and T3 in appropriate ranges
Pt advised about risk for thyroid storm; instructed to contact provider for new onset fever, agitation, tachycardia, irregular heartbeat, diarrhea, and/or pedal edema
Second most common cause of hyperthyroidism after Graves disease
Pathophysiology: Hyperplasia of thyroid follicular cells that no longer respond to regulation by TSH
Most common in elderly patients living in iodine-deficient areas, e.g. those surrounding the Great Lakes in the United States (chronic iodine insufficiency = increased risk for hyperplasia)
Most salt in the U.S. is iodized, but unprocessed Kosher or “sea salts” may not contain iodine
A single toxic adenoma is referred to as Plummer disease; it will present as a single area of accumulation on radioactive iodine uptake scan
Pt with h/o autoimmune disease s/p delivery presents with new onset episodes of palpitations and heat intolerance. Recently started on amiodarone, lithium. No goiter, thyroid tenderness, Graves' ophthalmopathy or pretibial myxedema on exam.
TSH > 0.1 mIU/L but < 0.4 mIU/L with elevated free T4 and T3 levels
Obtain anti-thyroperoxidase antibodies
Radioactive iodine uptake scan shows low uptake
Pt counseled that condition may progress to hypothyroidism
Pt encouraged to establish appointment with cardiologist and psychiatrist to discuss discontinuing amiodarone and lithium
Pt advised to follow-up for repeat TSH, FT4, and T3 testing in 6 weeks and again at 6 months
May be initiated by
Idiopathic autoimmune event (painless)
Childbirth (postpartum thyroiditis)
Medications, e.g. amiodarone, lithium
Categories of transient thyroiditis
Painless thyroiditis - May or may not be followed by hypothyroidism.
Hashimoto’s thyroiditis - Involves autoimmune destruction of thyroid gland that releases thyroid hormone; ultimately followed by hypothyroidism
Postpartum thyroiditis - Transient thyroiditis that occurs within 1 year postpartum
Diagnosis
Presence of anti-thyroperoxidase antibodies may indicate Hashimoto’s thyroiditis, but does not rule out Graves disease as they can be present in both conditions
A radioiodine thyroid scan may not be indicated in patients with a TSH > 0.1 mIU/L; follow-up with repeat laboratory testing is generally indicated
Pt with h/o recent viral illness presents with acute onset thyroid tenderness. Reports recent fever. Pain with palpation of thyroid and vesicular rash present on posterior pharynx/hand/feet on exam.
TSH > 0.1 mIU/L but < 0.4 mIU/L with elevated free T4 and T3 levels
Obtain anti-thyroperoxidase antibodies
Radioactive iodine uptake scan shows low uptake
Naproxen 500 mg BID for pain and inflammation
Pt cousled that condition generally improves at 6 weeks and resolves at 6 months
Pt advised to present for repeat TSH, free T4, and T3 testing in 6 weeks and at 6 months
Etiology
Inflammation due to viral illness releases preformed T4 and T3 hormone
Cases have been associated with Coxsackie disease, however, adults may not display the classic viral exanthem
Presence of anti-thyroperoxidase antibodies indicates autoimmune etiology, i.e. the condition is due to transient instead of subacute thyroiditis
Pt with h/o autoimmune disorders s/p neck surgery presents with tetany, seizures. Not actively seizing; reports recent paresthesias, emotional lability, anxiety/depression, and difficulty focusing. Hypotension, cataract, irregular heartbeat, positive Chvostek/Trousseau sign, lower extremity edema, and dry skin on exam.
Labs
CMP shows hypocalcemia with normal albumin
PTH level inappropriately low in the setting of hypocalcemia
Obtain repeat CMP; if repeat level is low
Obtain serum ionized calcium
Obtain serum 25-hydroxyvitamin D and magnesium levels to rule out alternate causes of hypocalcemia
EKG shows QTc > 500 milliseconds
Administer 2g calcium gluconate over 30 minutes; replete to corrected calcium level of 8.0 (see notes for further repletion options)
Etiologies
Most common: Parathyroid damage during neck surgery
Autoimmune destruction of parathyroid glands
Potential signs/symptoms of hypocalcemia include cataract, arrhythmia, refractory heart failure (edema), tetany, seizures, altered mental status
PTH and serum calcium
Corrected Ca = [0.8 x (normal albumin - patient's albumin)] + serum Ca
Normal PTH level = 10-65 mg/dL
Normal PTH in setting of low calcium also indicates hypoparathyroidism
Calcium repletion
1g calcium is equivalent to
CaCO3 250 mg PO
Calcium gluconate 1g IV over 30 minutes
Corrected calcium < 7.5 mg/dL with arrhythmia and/or seizure:
Start 2g IV calcium over 30 minutes
Notify ICU as transfer may be necessary if symptoms do not resolve. (Administering greater than 2g of calcium over 30 minutes requires a central line.)
Repeat CMP in 4 hours
Corrected calcium < 7.5 mg/dL with mild symptoms (e.g. paresthesias) and/or QTc > 500 milliseconds but no arrhythmia:
Obtain serum ionized calcium to confirm hypocalcemia
Administer 1g calcium (preferably PO) and repeat CMP in 12 hours
7.5 or greater and no symptoms: Consider starting 1g calcium carbonate PO and monitor with daily CMP
55 y/o F with h/o neck radiation, nephrolithiasis, long-bone fractures presents, bipolar disorder for health maintenance exam. Reports intermittent lethargy/fatigue, weakness, epigastric pain, nausea/vomiting, insomnia, and forgetfulness. Medications include lithium. Hypertension, irregular heartbeat, abdominal tenderness, flank pain, muscle weakness, and lower extremity edema on exam.
CMP shows hypercalcemia
Repeat CMP and re-evaluate serum calcium and creatinine levels
If repeat serum calcium elevated, obtain serum ionized calcium
Obtain serum vitamin D, magnesium, and lithium levels
PTH > 65 mg/dL in setting of hypercalcemia: Obtain 24-hour urine calcium:urine creatinine ratio
Ratio > 0.01: Primary hyperparathyroidism confirmed
Obtain Sestamibi scan to confirm hyperparathyroidism due to excess parathyroid activity and refer for surgical removal of parathyroid glands pending positive scan
Consider genetic analysis for MEN syndrome
Ratio 0.01 or less: Diagnose familial hypocalciuric hypercalcemia (see notes below)
Risk factors include female sex, age > 50 years, and h/o neck radiation
Presentation
Most patients are asymptomatic at diagnosis
Elements of the classic stones (nephrolithiasis), bones (osteitis fibrosa cystica), groans (abdominal pain due to pancreatitis), and psychiatric overtones (lethargy/fatigue, weakness, insomnia, impaired memory) may be present
Hyperparathyroidism is sometimes associated with hypertension, arrhythmia, heart failure, and muscle weakness
Diagnosis
Primary hyperparathyroidism is most commonly an incidental diagnosis
Low vitamin D and/or calcium levels may cause hypoglycemia and lead to elevated parathyroid hormone in the setting of low to normal calcium values
Lithium can raise PTH levels, thereby causing hypercalcemia; chronic use may also lead to renal failure and associated hypocalcemia due to decreased vitamin D production
Familial hypocalciuric hypercalcemia
This condition is due a “calcium sensor that reads low.” In other words, a normal sensor shuts off PTH when the calcium level reaches ~9.0 mg/dL, i.e. normal. In patients with familial hypocalciuric hypercalcemia, the sensor doesn’t activate until calcium levels reach ~11.0 or higher, i.e. elevated.
Patients may not need surgical removal of parathyroid glands if they are not displaying signs/symptoms of hyperparathyroidism
If PTH is low, primary hyperparathyroidism is ruled out: Obtain 25-hydroxyvitamin D, 1,25-hydroxyvitamin D, and PTH-rP level to evaluate for parathyroid-independent causes of hypercalcemia
Pt with h/o chronic kidney disease, bipolar disorder controlled with lithium, and h/o gastric bypass surgery presents with hypocalcemia. Reports recent paresthesias, emotional lability, anxiety/depression, and difficulty focusing. Hypotension, cataract, lower extremity edema, positive Chvostek/Trousseau sign, and dry skin on exam.
Labs
CMP shows hypocalcemia with normal albumin
Obtain repeat CMP
If repeat CMP shows hypocalcemia, obtain serum ionized calcium
PTH > 65 mg/dL
Obtain 25-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 levels
Obtain EKG and evaluate QTc
Start vitamin D and/or calcium supplementation as needed to prevent osteomalacia
Pt counseled about importance of vitamin supplementation s/p bariatric surgery
Etiology
Renal failure = most common etiology
May occur due to chronic lithium use
Decreases conversion of 25-hydroxyvitamin D3 to the active 1,25-dihydroxyvitamin D3
May be related to decreased vitamin D and/or calcium absorption, e.g. due gastric bypass surgery
Insufficient calcium intake is rare in developed nations
Normal values
PTH 10-65 mg/dL
25-hydroxyvitamin D > 10 ng/mL

OpenStax College / CC BY (https://creativecommons.org/licenses/by/3.0)
Patient with history of DM type 2, HTN, HLD, obstructive sleep apnea, non-alcoholic fatty liver disease presents due to weight gain. Patient is unhappy with her current weight. Does not exercise and reports inadequate fruit/vegetable consumption. Greater than 25% of calories consumed between evening meal and breakfast. Reports changes in routine leading to change in location where food is purchased, increased sedentary behavior, increased screen time, sleep deprivation. Medications include amlodipine, sulfonylureas, thiazolidinediones, amitriptyline, mirtazapine, paroxetine, antipsychotics. BMI > 30 kg/m^2.
Obtain TSH, HbA1c
Counseling
Diet
No diet has been shown to be superior for weight loss provided it reduces the number of calories consumed per day
Select a diet that is sustainable and, ideally, increases fruit and vegetable consumption
Reduce intake of beverages containing sugar, alcohol
Do not consume fewer than 800 Calories per day without medical supervision
Exercise: CDC recommends 150 minutes of moderate exercise per week including 2 days of strength training that work all major muscle groups
Additional risk factors for weight gain
Discount foods that often contain added sugar, salt
Night eating syndrome: Greater than 25% of calories consumed between evening meal and breakfast
Small changes in physical activity, e.g. energy saving appliances, decrease in vigorous physical activity by as little as 5-10 minutes per day
Increased screen time leading to sedentary behavior +/- inadvertent calorie consumption
Factors with minimal impact on overall weight (~5 pound weight gain or less): Healthy pregnancy, oral contraceptives
Initial interventions
Substitute weight neutral medications if possible (see notes)
Perform motivational interviewing concerning healthy lifestyle changes
Log calorie consumption and exercise habits x 1 week and follow-up to review results
Consider medical/surgical therapy (see below) after instituting lifestyle change and ruling out other medical disorders (see below)
Polycystic Ovarian Syndrome (PCOS)
Cushing disease
Physical exam: Facial erythema, buffalo hump, abdominal stretch marks, bruising, and thin arms/legs
Verify no exogenous glucocorticoids
Concern for diagnosis per physical exam: Obtain 24-hour urinary free cortisol (UFC) excretion x 2 measurements
Binge eating disorder
Criteria (DSM 5)
Recurrent and persistent episodes of binge eating associated with three (or more) of the following: Eating much more rapidly than normal, eating until feeling uncomfortably full, eating large amounts of food when not feeling physically hungry, eating alone because of being embarrassed by how much one is eating, feeling disgusted with oneself/depressed/very guilty after overeating
Marked distress regarding binge eating
Absence of regular compensatory behaviors (such as purging)
Treatment
Refer for counseling
Start escitalopram 10 mg daily and increase to 20 mg daily after 1 week
BMI > 30 with < 5% weight loss after 6 months: Consider oral therapy
History of DM: Start liraglutide 0.6 mg sub-Q daily and increase dose by 0.6 mg at weekly intervals until reaching maximum dose of 3 mg qd
No history of DM and
No cardiovascular risk factors: Start phentermine-topiramate 3.75-23 mg daily x 14 days. Increase to 7.5-46 mg daily x 12 weeks before re-evaluating weight loss. Discontinue if < 3% weight loss during that time.
Cardiovascular risk factors: Start lorcaserin 10 mg BID and re-evaluate after 12 weeks. Patient counseled about risk of anal leakage with medication.
BMI > 40: Discuss referral to bariatric surgery program
Obesity classification based on BMI (kg per m^2): Class 1 (30.0-34.9), Class 2 (35.0-39.9), Class 3 (40 or greater)
Complications of obesity include DM type 2, HTN, HLD, obstructive sleep apnea, non-alcoholic fatty liver disease
Medication classes associated with weight gain and alternatives
Antidepressants
Promote weight gain: Amitriptyline, mirtazapine, paroxetine
Weight neutral: Most SSRIs, e.g. escitalopram, fluoxetine
Promote weight loss: Bupropion
Weight neutral antipsychotics: Aripiprazole (Abilify), haloperidol, and ziprasidone (Geodon)
Mood stabilizers: Lithium promotes weight gain while oxcarbazepine is weight neutral
Blood pressure agents: Amlodipine promotes weight gain while ACE inhibitors are weight neutral
Treatment
Consider drug therapy in the following cases
BMI of 30 or greater
BMI of 27 or greater with cardiovascular comorbidities
Failure to lose 5% of total body weight after 3-6 months of comprehensive lifestyle change
Weight loss medications
Phentermine-topiramate has greater efficacy that lorcaserin or liraglutide but comes with increased cardiovascular risk.
Orlistat 120 mg TID with fat-containing meals is another option with efficacy similar to that of lorcaserin; drawbacks include anal leakage. Patients should avoid wearing white pants when taking the medications.
Bariatric surgery (see below)
Bariatric surgery
Without bariatric surgery, annual probability of achieving BMI < 30 in patient with BMI 40 to 44.9 is 1 in 1290 for men and 1 in 677 for women (JAMA 2017)
Relatively safe and reduces obesity-related conditions, e.g. all-cause mortality, myocardial infarction, stroke
Post-surgical care
Bariatric multivitamin, ferrous gluconate 240 mg [elemental iron 27 mg] daily
Evaluate for nutrient deficiencies every 3 months for 1 year and then yearly: Obtain CBC, TIBC, ferritin, B1, B12, folate, 25(OH) vitamin D, zinc, copper
5 y/o M with h/o prolonged candida infections presents with acute onset lethargy, polyuria, and polydipsia. Parents report family h/o DM type 1. Weight loss noted on exam.
Labs
Urine positive for ketones
BMP shows plasma glucose > 200 mg/dL
Positive autoantibodies to islet cells, insulin, glutamic acid decarboxylase, insulinoma-associated antigen-2, and zinc transporter 8
Obtain TSH to screen for concomitant thyroid disease; if abnormal test for antithyroid peroxidase and antithyroglobulin antibodies
Treatment
Stabilize pt according to DKA protocol
Initiate basal insulin glargine at 0.1 u/kg/day and follow-up fingersticks in 1 week; increase dose by 10% weekly until morning fingerstick glucose consistently < 130 but > 90 u/dL
Start 0.1 u/kg/day short acting insulin aspart divided between breakfast, lunch and dinner; adjust by 10% weekly until preprandial fingerstick glucose < 130 but > 90 u/dL
Education
Parents and pt educated about insulin injection
Parents and pt educated about pre-meal and pre-bedtime fingerstick glucose monitoring with goals of 90-130 mg/dL and 90-150 mg/dL, respectively
Parents counseled that failure to adhere to insulin regimen may result in blindness, heart/vascular disease, kidney failure, and/or limb amputation
Follow up as outpatient
Monitor for development of HTN
Consider starting lisinopril if urine albumin-to-creatinine ratio > 30 mg/g
Starting at age 10 years
Obtain lipid profile; start statin if LDL > 160 mg/dL
Perform yearly foot exam
Refer for yearly ophthalmology exams
Consider referral for insulin pump
Onset has a bimodal distribution with peaks occurring at age 4-6 years and 10-14 years
HbA1c
HbA1c may be inaccurate if onset occurred fewer than 3 months ago; obtain BMP
Long term HbA1c goal in pediatric patients is less than 7.5%
Increased risk for other autoimmune diseases:
Consider screening for Celiac disease if presenting with diarrhea
Also consider Addison’s disease, autoimmune hepatitis, and/or myasthenia gravis if associated symptoms develop
Renal disease
Monitor for development with yearly urinary albumin-to-creatinine ratio
Most common cause of hypoglycemia in previously controlled DM I

Acanthosis nigricans
Non-caucasian patient < 65 years with h/o schizophrenia, NAFL, PCOS, gestational diabetes presents for health maintenance exam. ROS positive for fatigue, blurry vision, polyuria/polydipsia, and numbness/tingling in the lower extremities. BP > 140/90, acanthosis nigricans, and foot ulcer on exam.
Initial Labs
No h/o asplenia, anemia, or recent acute blood loss with HbA1c > 6.4%
Obtain lipid panel
HbA1c and Associated Therapy
HbA1c < 9%
GFR > 30: Start metformin and recheck HbA1c every 3-6 months
If follow-up HbA1c > 7%, add up to 2 additional oral agents before starting insulin (see HbA1c > 9%)
HbA1c 9-10%: Initiate metformin and empagliflozin (Jardiance); pt counseled about risk for UTI/pancreatitis and need for repeat HbA1c in 3 months
HbA1c > 7% after 3 months: Start liraglutide (Victoza) and recheck HbA1c in 3 months
HbA1c > 7% after 3 months on 3 oral agents: Start insulin (see HbA1c > 10%)
Initial HbA1c > 10%
Initiate basal insulin glargine (Lantus) at 0.1 u/kg/day
Initiate finger-stick log and follow-up in 1 week
Increase dose by 10% weekly until morning fingerstick glucose consistently < 130 but > 80 mg/dL
Titrate to to 0.4-1.0 u/kg/day until morning fingerstick goals are achieved and decrease by 10% for hypoglycemic events (morning fingerstick < 70)
If HbA1c > 7% after 3 months: Start 0.1 u/kg/day short acting insulin aspart (Novolog) divided between breakfast, lunch and dinner (e.g. 120 kg = 12u = 4u at each meal). Adjust by 10% weekly until preprandial fingerstick glucose < 130 but > 80 mg/dL.
Monitor HbA1c every 3-6 months
Obtain microalbumin-to-creatinine ratio and perform foot exam yearly
Additional Treatment
Stain therapy
ASCVD < 7.5%: Start rosuvastatin 10mg
ASCVD > 7.5%: Start rosuvastatin 20mg
Administer pneumococcal vaccine (PPSV23)
Counseling
Refer pt for intensive behavioral counseling interventions focusing on diet/exercise
Pt advised that failure to adhere to therapy may result in blindness, cardiovascular disease, kidney failure, and/or limb amputation
Patients at increased risk for developing diabetes
Member of ethnic groups including Asian, black, Hispanic, Native American/Pacific Islander
Use of antipsychotics
HbA1c value of 5.7 to 6.4% (“pre-diabetes”)
Screening
Screen patients age 40 to 70 years who with BMI 25.0 or greater; repeat every 3 years if results are normal
Screening may be considered in patients under 40 with BMI > 85th percentile or those with risk factors such as ethnicity, family history, PCOS, HTN, and/or HLD
Positive screen includes one of the following
HbA1C level > 6.4%
Fasting plasma glucose 126 mg/dL or greater
Plasma glucose 200 mg/dL or greater for fasting level and/or 75 g 2-hour glucose tolerance test
HbA1c
HbA1c goals
Age less than 65: Goal < 7.0%
Age 65 or greater: Goal 7.0 to 7.9%
HbA1c assumes RBC lifespan of approximately 3 months
Falsely low values occur with hemolytic anemias, acute blood loss
Falsely elevated values occur with asplenia, iron deficiency/aplastic anemias
Cannot be used in pregnancy (see gestational DM)
Fingerstick glucose goals
Home
Morning fingerstick glucose: 70-100 mg/dL
Preprandial: 80-130 mg/dL
Hospital fingerstick glucose: 140-180 mg/dL
Non-insulin medications
Metformin
Contraindicated in patients with GFR < 30 mL/minute/1.73 m^2
Once initiated, should be continued as long as tolerated; additional agents including insulin should be added to metformin (ADA Guidelines)
May lower B12; check levels periodically, especially if anemia or peripheral neuropathy develops
If empagliflozin or liraglutide not tolerated, start pioglitazone
See DM type 2 medications for more information
Pt with h/o DM type 1 presents with sub-acute onset of polyuria/polydipsia with concomitant weight loss, fatigue, dyspnea, N/V, abdominal pain, polyphagia. Reports recent pneumonia, UTI, cocaine/alcohol abuse. Medications include second generation antipsychotics. Has not been taking insulin as instructed due to pump failure, financial issues, confusion about insulin regimen. Febrile and stuporous with dry mucous membranes on exam. Initial labs show serum bicarbonate < 18 mEq/L, glucose > 250 mg/dL, anion gap (AG) > 16 mEq/L, serum osmolality > 320, pH on ABG < 7.3.
Labs
Obtain CBC, CMP, ABG, U/A
Obtain serum beta-hydroxybutyrate, amylase, lipase, lactic acid, creatinine kinase
Obtain HbA1c if not performed within previous 3 months
Timed
Obtain BMP, phosphorus, magnesium q4 hours until AG < 12
Obtain fingerstick glucose q1 hour x 4
Report intake and output q4 hours
IV fluid
Initial progression
Normal saline (0.9%) at 1 L/h x 1h, then 500 mL/h x 2h then
0.45% saline at 500 mL/h x 2h then
0.45% saline at 200 mL/h maintenance
When WBG < 250 mg/dL, start D5 0.45% saline at 200 mL/hr
If initial potassium
4 to 5.2: Infuse KCl at 10 mEq/h IV x 2h
3.3 to 4: Infuse KCl at 10 mEq/hr IV x 3h
3.2 or lower: Replete as appropriate and start KCl at 10 mEq/hr IV x 3h
Insulin
Start insulin infusion at 0.1 u/kg/h; max 10 u/h
When WBG < 250 mg/dL and decreased 100 mg/dL from starting value, decrease infusion rate by half and recheck WBG in 30 min
When WBG < 200 mg/dL and decreased 60 mg/dL in previous 2 hours, decrease insulin rate by half
When WBG <100mg/dL, decrease insulin rate by half and change to D10 0.45% saline at current rate
Administer long-acting insulin SQ when AG < 12 and serum CO2 > 14
Continue insulin infusion for 30 minutes after starting long acting insulin
Additional evaluation and treatment
Obtain EKG
Zofran 4 mg IV q8h PRN for nausea
Monitor for s/sx of cerebral edema
Pt's family advised that fatality rate is up to 5%
Educate pt and family about insulin adjustment during illness, blood glucose monitoring, and importance of medication compliance

Simplified management algorithm. See above for full details.
Febrile illness precedes 40% of DKA cases
AG = anion gap = Na - (Cl + CO2)
Serum osmolality = 2(Na + K) + (glucose/18) + (blood urea nitrogen/2.8)
Bicarbonate therapy is has not be shown to improve outcomes
Rule out
10-15% of DKA patients have concomitant pancreatitis; rule in/out with serum amylase, lipase
Other high anion-gap metabolic acidosis, e.g. lactic acidosis, uremia, rhabdomyolysis, toxic alcohol ingestion (alcohol, ethylene glycol, methanol)
diagnosis = serum glucose >600, osmolarity >300, absent/minimal ketonse, arterial pH>7.3, serum bicarb>20
-high flow NS; add dextrose 5% when WBG <200
-serum potassium <= 5.2; add IV potassium
-serum potassium >=3.3; start initial continuous insulin infusion
-consider bicarbonate if pH < 6.9
-consider phosphate for serum phosphate <1.0 mg/dL, cardiac dysfunction, respiratory depression
-frequent monitoring of serum Ca
-tolerates PO intake, WBG<200mg/dL, anion gap<12 and serum HCO3 >15; d/c start SQ basal bolus insulin and d/c IV insulin in 1-2 hours
(true for DKA as well)
45 y/o F with h/o smoking presents with pain/stiffness in the proximal interphalangeal/metacarpophalangeal joints, wrists, and knees. Reports fatigue, weight loss, dry eyes, dry mouth, SOB, and morning stiffness in affected joints lasting greater than 1 hour. Denies distal interphalangeal joint pain, lumbar spine pain. Reports family h/o rheumatic disease, including RA. Conjunctival injection, joint swelling of PIPs, and rheumatoid nodules on exam.
Obtain ESR, CRP, IgM rheumatoid factor, and anti-citrullinated protein antibody level
Obtain CBC to rule out anemia
Screen for hepatitis B/C and tuberculosis if not already performed
Treatment
Start methotrexate 10 mg once weekly; increased by 5 mg every 4 weeks to maximum dose of 20 mg once weekly
Symptom resolution not achieved with 20 mg weekly; refer to rheumatology
Pt informed that DMARD may be tapered or discontinued once 6 months of symptom remission is achieved
Pt counseled that symptom remission with methotrexate monotherapy is only achieved in approximately 40% of patients
Earlier diagnosis and treatment of RA with disease-modifying antirheumatic drugs (DMARDs) dramatically improves outcomes
Mean age at onset: 48 years
Rheumatoid nodules and radiographic erosive changes are no longer criteria for diagnosis
Differential includes systemic lupus erythematosus, systemic sclerosis, psoriatic arthritis, sarcoidosis, crystal arthropathy, and spondyloarthropathy
Extra-articular manifestations
Include keratoconjunctivitis sicca, interstitial lung disease, and pleural effusions
May manifest as complaints of eye redness, dry eyes, dry mouth, and/or SOB
Methotrexate
Patients must be screened for hepatitis and tuberculosis before starting DMARDs
Toxicity risk increases with doses greater than 20 mg weekly
70 y/o white F with h/o carpal tunnel syndrome presents with gradual onset b/l pain in shoulders, neck, and hips. Reports fatigue, weakness, low-grade fever, morning stiffness lasting >45 minutes, and myalgias/arthralgias that are worse at night. Denies abrupt onset headache, tongue/jaw claudication. Weight loss, proximal joint pain, proximal muscle weakness, asymmetric arthritis in wrist/knees, pitting edema of wrists/ankles on exam.
Labs
ESR > 40 mm/hr
CBC shows mild anemia, thrombocytosis
Obtain CMP, TSH, CRP, creatinine kinase, rheumatoid factor, urinalysis, and protein electrophoresis to rule out mimics, including paraneoplastic syndrome
Obtain DEXA scan prior to starting corticosteroid therapy
Treatment
Start prednisone taper: 15 mg qd x3 weeks, then 12.5 mg qd x3 weeks, then 10 mg qd x5 weeks, then decrease by 1 mg every 5 weeks as tolerated
Pt on long-term corticosteroid therapy: Prophylax with alendronate 35 mg q weekly to preserve bone mineral density and reduce fracture risk
Pt counseled that the average length of treatment with steroids is 2 years and that relapses requiring repeat courses may occur
Pt counseled about long-term risks of corticosteroid use including peptic ulcers and loss of bone mineral density
Most common chronic inflammatory condition in older adults
Affects ~1 in 140 people of European descent >50 y/o
Giant cell (temporal) arteritis
Occurs in up to 25% of polymyalgia rheumatica cases
Red flags: Sudden onset headache, jaw/tongue claudication, ESR >100 mm/hr
Treatment: Prednisone 60 mg qd, ophthalmology consult +/- temporal artery biopsy
Associated tenosynovitis may produce carpal tunnel syndrome
45 y/o F pt with h/o atopy presents with gradual onset muscle weakness. Weakness particularly noticeable when climbing stairs, rising from seated position, and/or picking up heavy objects, e.g. groceries. ROS positive for dysphagia, SOB. Physical exam reveals faint pulmonary crackles, proximal muscle atrophy/weakness affecting deltoids/hip flexors, hyperkeratotic/fissured skin on palmar surfaces (mechanic’s hands). [Gottron’s papules, heliotrope eruption present.]
Labs
Obtain CBC, CMP, creatine kinase (CK) and lactate dehydrogenase (LDH) levels
Obtain antinuclear antibodies; if positive
Obtain anti-Jo-1 antibodies
Consider obtaining anti-Ro, anti-La, anti-Sm, anti-RNP antibodies
Concern for heart disease: Obtain CK-MB
Imaging
EKG shows non-specific conduction abnormalities
CXR shows interstitial opacities suspicious for interstitial lung disease
MRI shows widespread muscle inflammation, fibrosis, calcification
Muscle biopsy shows lymphocytic infiltrate
Treatment: Refer/consult rheumatology
Unstable: Admit to hospital, start methylprednisolone IV 1000 mg/day
Stable
Start 1 mg/kg prednisone daily (max dose 80 mg/day)
Consider transitioning to azathioprine 50 mg/day for long-term therapy
Pt counseled about risks of immunosuppressive therapy

Author: Elizabeth M. Dugan, Adam M. Huber, Frederick W. Miller, Lisa G. Rider

Author: Elizabeth M. Dugan, Adam M. Huber, Frederick W. Miller, Lisa G. Rider
Prevalence = 2 in 100,000
Skin changes
Nonspecific findings, e.g. mechanic’s hands occur in both disorders
Shawl sign: Poikiloderma in sun exposed areas (e.g. upper back, chest) sometimes found in dermatomyositis patients
Gottron’s papules/heliotrope eruptions are pathognomonic for dermatomyositis
Gottron’s papules: Symmetrical violaceous lesions on extensor surfaces
Heliotrope eruption: Symmetrical violaceous eruption on the upper eyelids
Additional clinical manifestations
Interstitial lung disease affects 10% of patients
Damaged cardiac muscle may produce conduction abnormalities on EKG
Dysphagia may occur due to oropharyngeal muscle weakness
Diagnostic testing
Presence of anti-Ro, anti-La, anti-Sm, or anti-RNP antibodies may indicate presence of other autoimmune conditions
MRI is sensitive, but not specific
Muscle biopsy showing perifascicular atrophy is pathognomonic for dermatomyositis